[Editor's note: This is third in a series of in-depth audio reports and text articles investigating the state of Vancouver drug policy 13 years after the ground breaking Four Pillars approach was adopted. The project is a partnership between The Tyee and the University of British Columbia's documentary radio series, The Terry Project on CiTR.]
In 2001, Vancouver launched The Four Pillars, a new approach to dealing with drug dependency. Those pillars were prevention, enforcement, harm reduction and treatment. The architects of the Pillars sought support from all levels of government for their guiding principle: that drug addiction should be understood as a medical problem that can be managed, not a moral problem that should be policed.
Methadone, within such shifted thinking, loomed large.
Methadone is a synthetic opiate, which doctors can prescribe as a substitute for heroin. Like heroin, it is highly addictive, but it has a much longer half-life. Which means that its users, free from constant heroin withdrawals, report leading more stable lives. Importantly, methadone users also have more contact with health professionals than heroin users and do not have to participate in a dangerous black market.
Methadone, like much of the Four Pillars' recommendations, is pragmatic. Proponents say that it is dangerous and irresponsible to demand that all drug users immediately and permanently abstain from illicit drug use.
The Four Pillars called for an expanded methadone program. Today British Columbia's health authorities consider methadone maintenance treatment, or MMT, the 'gold standard' for treating opioid users. Patients of MMT go to a methadone dispensing pharmacy once per day to ingest the synthetic opioid.
But the patchwork of regulated and unregulated treatment facilities in and around Vancouver is no testament to the triumph of medicalized methadone. As we learned while exploring that fragmented and polarized world, methadone is either a benevolent life saver, or an evil killer. It depends on who you ask.
Jim O'Rourke falls into the second camp. Talk to the executive director of Vision Quest Society about methadone and he shows you a picture of hollow-eyed prisoners of Nazi concentration camps, and asks you to compare these images to the men and women standing in line at a methadone clinic.
"That's what they fed them when they walked all the Jews into the gas chambers," he claims, "they were loading them up with methadone. Sure as God made green little apples. And how you tell that is the eyes. The eyes never lie."
While there is no proof that the Nazis used methadone for these purposes, O'Rourke is not some marginal oddball. His organization operates five residential drug recovery homes in the Lower Mainland and plans to open two more, including a 100-bed treatment facility. Which makes O'Rourke one of the largest drug treatment providers in British Columbia, if not the largest.
Indeed, 13 years since Vancouver passed The Four Pillars, much of the drug treatment community still rejects its core philosophy.
Our investigations also revealed a wide disparity in the approaches, resources and levels of regulation among drug treatment options in the Lower Mainland -- a welter of variables facing a person wanting to escape, or at least lessen, the misery of their drug dependency.
This third article in our series examining the state of the four pillars for The Tyee and The Terry Project on CiTR turns to drug treatment in the Lower Mainland.
You can hear the documentary radio instalments that accompany this series by clicking on the play icon below. Or you can subscribe to the series on iTunes.
Pushed and pulled
Jim O'Rourke claims that the provincial government thinks of heroin users in the same way as the terminally ill. For him, when a doctor puts a patient on a methadone maintenance program, it does not treat their problematic relationship to heroin -- it condemns them to death.
Although O'Rourke's views may seem extreme, he is not alone in his condemnation of methadone. A significant portion of the drug treatment community vehemently opposes methadone and several other programs recommended by The Four Pillars.
Susan Sanderson of the Realistic Success Recovery Society, which manages three homes, also refuses methadone clients.
"If you're using methadone you're stoned," says Sanderson. "How can you possibly do a program? We tried it. We had some residents who were here on methadone. They just sat in the corner and drooled."
Sanderson claims that doctors are too quick to treat addiction with methadone. Like O'Rourke and other recovery home managers, her programming follows abstinence-based, 12-step principles.
Sanderson and O'Rourke, like many of British Columbia's licensed treatment providers, have minimal formal training, but immense personal experience. O'Rourke was a drug trafficker with a heroin dependency. Sanderson's husband developed a cocaine dependency.
The other side of the debate tends to be represented by psychiatrists, physicians, nurses and public health officials who stress pragmatism over absolutism.
When a drug user enters the world of drug treatment, they are pushed and pulled by these competing views. Depending largely on circumstance, they will end up in either a government-run treatment centre, a community care facility, an assisted living facility, or an unlicensed recovery home. Each of these four categories of treatment fall under different regulatory frameworks, offer different treatment philosophies and provide different standards of care.
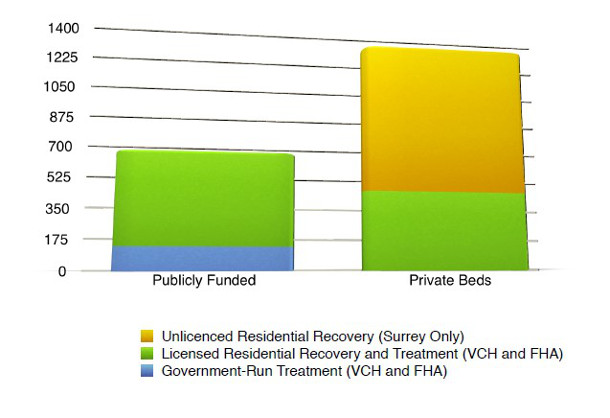
Combined, the Provincial Health Services Authority (PHSA) and the Vancouver Coastal Health Authority (VCHA) provide 130 government-run drug treatment beds in Vancouver and Burnaby: 30 at B.C. Women's Hospital, and 100 at the Burnaby Centre for Mental Health and Addictions.
The Burnaby Centre for Mental Health and Addictions accepts patients from all over BC who have repeatedly failed with local treatment options. All patients must have dual-disorders, meaning a mental disorder and a substance use disorder.
Dr. Schütz is a researcher and a clinical psychologist at the centre. The Tyee meets Dr. Schütz in his office, where there is a Pfizer leaflet tacked to his push board, and a joystick next to his desk. The joystick is for a computer game that he has prepared for his patients.
"It's really simple. It's so simple it might be concerning," he says. "Individuals are exposed to cues on the computers. Cues like cigarettes. They just have to push it away. Other cues, like pencils or apples, they have to pull them in."
Dr. Schütz believes that addiction has a less to do with consciousness decision-making and more to do subconscious impulses. By training his patients to automatically resist certain cues on the computer game, he hopes that they will be less likely to relapse in the real world.
The Centre conducts these sorts of research projects in order to expand and improve on their treatment programming.
As Dr. Schütz gives a tour of the facility, he describes their 60+ programs -- from cognitive behavioural therapy, to groups for those diagnosed with PTSD, to female empowerment groups.
The halls are grey, but someone has painted palm trees all over them. Dr. Schütz says he thinks the building used to be a juvenile detention facility, and the trees were an effort to make it seem "less institutional."
Downstairs, Dr. Schütz walks through a large recreational room and into a smaller room filled with musical instruments. Inside, a musical therapist is preparing guitar lessons and a music appreciation classes.
The Centre provides the latest in evidence-based drug treatment, he says, but it also provides drug treatments that are not evidence-based -- like yoga, acupuncture, or art and music therapy.
Dr. Schütz says that these activities can be empowering, but he stresses the centre's medical treatments.
"Methadone has been very clearly shown to improve individuals' health substantially," says Dr. Schütz. "Individuals do stop using heroin. They become more socially functional. They reduce illegal activity."
Dr. Schütz says that methadone stabilizes his patients, which helps to keep them in treatment. If they ask to be tapered off methadone, Dr. Schütz usually slows the process down. He says that patients are less likely to relapse if they stay on the program longer.
In B.C., 40.5 per cent of clients on the program stay in the program for at least 12 months, according to the most recent report on the program, citing figures from 2005. That figure of four out of ten is around the North American average, but significantly below the retention rates in Ontario, according to the report.
There is an overwhelming body of research on the methadone maintenance program that claims patients have better treatment outcomes if they stay in the program longer.
"That's bullshit. That's doctor's talking. That's what they do," says David Berner, who opposes methadone. "I don't believe it's a medical problem. I've seen very few medical people help addicts."
Berner is the director of the Drug Prevention Network of Canada, an organization that solicits donations and preaches abstinence. He claims The Four Pillars was a PR stunt. The only pillar that mattered was harm reduction, he argues; the other three -- prevention, treatment, and enforcement -- are not pillars, but toothpicks.
Berner is persuasive and charming. He describes himself as a simple boy who never had the temperament for academia. "I'm sorry I have these weird old values. It would never occur to me to walk across the street and hand a drunk a shot glass. If my daughter was cutting her wrists, it would never occur to me to sterilize the razor blade."
Berner founded B.C.'s first residential treatment program in 1967. Today, he serves as a therapist for Orchard Recovery Drug Treatment Centre on Bowen Island.
Residential Treatment: The Community Care Facility Model
Residential treatment facilities like Orchard Recovery fall into three descending levels of regulatory scrutiny.
"There are a very complex set of standards," says Brenda Plant, executive director of Turning Point Recovery Society. "Everything from how big the bedrooms are to food you are serving to the level of safety in the house. Pretty much everything we do corresponds to a standard in the Community Care and Assisted Living Act."
Turning Point is one of five adult treatment centres in Vancouver that is registered as a community care facility. There are three registered in Surrey.
Turning Point benefits from a number of financial incentives that are only available to homes at their level accreditation. They are able to bill the Ministry of Social Development and Social Innovation $40 per day for each of their clients on social assistance. Additionally, they are able to cover a number of their beds through contracts with government agencies, including BC Housing, WorkSafeBC, and Vancouver Coastal Health.
With those resources, Turning Point provides a high standard of care. They have a large staff that offers a wide array of personalized treatments and services.
However, these five community care facilities have limited capacities. Plant says that Turning Point always has at least 15 people on the waitlist for their 22 beds. The last person on the list can wait for 14 months or longer.
Typically, five of Turning Point's 22 beds are funded by VCH. Currently, they have no VCH beds. However, a VCH spokesperson said it has nothing to do with their standard of care, but simply that Turning Point missed a recent deadline to renew their contract.
Residential Treatment: Assisted Living Model
Vancouver drug users are more likely to end up in an assisted living residence than a community care facility. There are 38 assisted living residences in the lower mainland, providing 279 drug treatment beds. All 279 beds are paid for privately, typically through the client's social assistance.
Although still licensed under the Community Care and Assisted Living Act, these facilities follow less stringent standards. For instance, a community care facility would typically have a dietician approve the house menu, while an assisted living residence would not.
O'Rourke's Vision Quest houses are licensed as assisted living residences. Vision Quest provides a high standard of care, but -- like the overwhelming majority of assisting living residences -- their treatment program is abstinence-based, rejecting methadone.
The Tyee was able to reach 29 of 38 licensed residential recovery centres in the Lower Mainland, which are mostly in Surrey. Of those 29, five accepted methadone clients. Twenty-four did not accept any methadone clients or only accepted methadone clients with very low doses who are already committed to quickly weaning themselves off.
Not all declared an approach, but more than two thirds of them, 26, were avowedly abstinence-based using 12-Step programs.
At the Burnaby Centre for Mental Health and Addictions, Dr. Schütz treats some clients with abstinence-based programming, and others with methadone. He says that treatment providers should be flexible, not dogmatic.
"For some individuals, abstinence-based is definitely the best treatment. And for others, they are simply not able to do it," he says. "If you are very inflexible and you say the only goal can be abstinence, then you will kind of select those that are doing the best and forget about the mass of people."
The world of the unlicensed recovery homes
The majority of recovery homes are not licensed under the Community Care and Assisted Living Act. These homes face little regulatory scrutiny, making it difficult to know their treatment philosophy or standard of care.
These homes have a notorious reputation for having poor living conditions, substandard meals, and unscrupulous managers with connections to questionable methadone pharmacies.
In 2010, CTV News and Jim O'Rourke exposed agents of one pharmacy offering Vision Quest a $100 per month per client kickback. In May of this year, The Province connected George Wolsey, the disgraced ex-pharmacist, to a Surrey pharmacy that was serving unlicensed recovery homes
Multiple treatment providers estimate there were around 200 unlicensed recovery homes. Then, in July of this year, the City of Surrey said it shut down 114 of the most problematic houses.
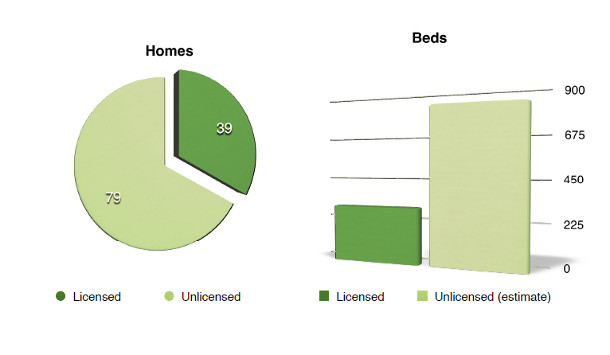
According to leaked documents obtained by The Tyee, the City of Surrey is aware of at least 119 unlicensed recovery homes that continue to operate as of July 2014. The documents count 569 beds in 54 of the 119 homes.
Jas Rehal, Surrey's bylaw manager, confirmed the authenticity of The Tyee's documents. However, he claims that the numbers have changed since July, and Surrey is now aware of 79 unlicensed recovery homes. Rehal says that the RCMP has active investigations into 17 of those homes.
Using the average number in the 54 homes (10.54), The Tyee estimates that there are approximately 832 beds in the remaining 79 homes.
Despite the various concerns, Dr. Schütz says that many drug users are helped by the private drug recovery industry. However, he wishes there were more government-run, evidence-based treatment beds.
"On the other hand, as long as the number is relatively small, and as long as the health care system is not willing to push in this direction," says Dr. Schütz, "this is for a lot of people the best option still."
Vancouver Coastal Health and Fraser Health provided The Tyee with a breakdown of all publicly funded beds within their respective jurisdictions. Combined, those numbers are still lower than The Tyee's estimate for Surrey's unlicensed recovery homes.
In September of last year, Gregor Robertson's mayor's taskforce on mental health and addictions recommended the provincial government create an additional 300 long-term mental health and addiction treatment beds, but the province has not acted on that recommendation.
Next week: An update on the third of the Four Pillars: the controversial concept of harm reduction. ![]()
Read more: Health, Municipal Politics

















Tyee Commenting Guidelines
Comments that violate guidelines risk being deleted, and violations may result in a temporary or permanent user ban. Maintain the spirit of good conversation to stay in the discussion.
*Please note The Tyee is not a forum for spreading misinformation about COVID-19, denying its existence or minimizing its risk to public health.
Do:
Do not: